
Dr. Luis Javier Roca Ruiz
EFORT engaged with Dr. Luis Javier Roca Ruiz of the department of orthopaedics and traumatology at Virgen Macarena University Hospital in Seville, Spain to discuss his positive views of preventive analgesia and the role it plays in avoiding the chronification of acute pain and reducing the risks of disability. During our discussions, Roca Ruiz provided examples of his practical experience using total knee arthroplasty as a baseline for the conversation, but the principles he discusses are ones he believes should be applied in any surgical context, addressing pain management well before the first incision and throughout the postoperative pain management regimen.
This article is part of our continuing series to raise awareness of the unmet needs in postoperative pain management (POPM) and to develop solutions that improve POPM across Europe. The opinions expressed in this interview are meant as an informal conversation to facilitate dialogue.
Separate the ‘good’ from the ‘great’ in orthopaedics and traumatology
Acute pain chronification is a challenge that, for better or worse, all orthopaedic surgeons and traumatologists must address. Roca Ruiz notes that in his estimate, one in 10 patients will encounter chronic pain symptoms following surgery and he separates “good” practitioners from “great” practitioners with a simple test. “Good” surgeons, according to Roca Ruiz, are those who are experts in precision performance during the surgical procedure: providing minimally invasive incisions; respect for soft parts; nominal use of the electric scalpel; keeping the surgical saw in good upkeep; and other factors routinely in place for the surgical practice. Those who are “great” manage patient care from a wholistic perspective, acknowledging the long-term effects of their intervention and being a leader among a team of professionals including nurses, physical therapists, anesthetists, and others using pre-surgical, surgical and the immediate post-surgical timeframe to maximise patient satisfaction and to improve clinical results.
Roca Ruiz finds preventive analgesia to be key to this wholistic approach. It is one thing, he postulates to simply reduce postoperative pain, which in his estimate is the responsibility of all good practitioners working in tandem with the pain management team. To carry pain management into the next level and to overcome chronic pain, preventive analgesia should be combined with surgical pain management throughout the patient’s surgical journey, including social care and other supports as appropriate with early evaluation of the patient’s pain and mobility profile.
A measure of success
Using TKA as his basis, through early intervention with preventive analgesia as part of the full spectrum of surgical patient care, Roca Ruiz points to lower post-surgical VAS scores and increased joint function as important markers of the benefit of preventive analgesia. By managing preoperative pain with early analgesic administration, practitioners like Roca Ruiz seek to influence postoperative results by decreasing the onset of central sensitization so that nociceptive input is blocked early from influencing the central nervous system. While it may seem counterintuitive, providing increased preoperative analgesia reduces the overall use of analgesics later in the postoperative phase of the patient’s surgical journey, not only in the first 24 hours when early mobilization is a key factor, but also in the days following the procedure. As long-term pain and continued use of analgesics can negatively impact patient satisfaction with a surgical procedure as well as overall patient outcomes, addressing these issues preoperatively and perioperatively should increase patient satisfaction, showing improved VAS scores and mobility with the potential to reduce the long-term use of postoperative analgesia: important steps in addressing the risk of acute pain chronification.
Roca Ruiz explains that there are regularly varying levels of patient satisfaction with their surgical encounter and pain management. Often these issues involve the patient’s overall expectations of the procedure, such as time to recovery and exaggerated hopes of improved function. Frequently, however, patients’ postoperative issues are centered around ongoing acute pain following the procedure. Similar to the way a health care professional would manage a patient’s expectations of a surgical result with early intervention in the form of patient education, preventive analgesia is a method of addressing postoperative pain with early intervention. The results are generally that patients have a reduced postoperative use of analgesics, as well as improved function, shorter hospital stays and better overall patient satisfaction.
According to Roca Ruiz, positive implications of preventive analgesia also persist in the long term, as reductions in pain facilitate a return to function, which in turn reduces issues surrounding atrophy and the risk of disability and pain chronification over time. When pain becomes less of a postoperative issue for the patient, it allows nursing to better focus on other patient management issues, and the attending physician has a potential for clearer follow-up when seeking early detection of other complications of the procedure.
Controversy
To Roca Ruiz, the benefits he has seen in his practice outweigh some of the controversy and confusion around preventive analgesia and some of its perceived scientific merits. Risk factors to the patient, for example, do not step beyond what Roca Ruiz considers the normal standard of care for any other practice. For example, he notes that special care should be taken when matching preventive analgesic treatment options to the risk factors associated with the patient. This is especially true, for example, when dealing with risks of bleeding, as early intervention with pharmacological pain management could influence intraoperative and postoperative bleeding issues, depending on the pharmacological agent involved and the patient risk factors. Beyond these risks, however, Roca Ruiz points out that preventive analgesia might also assist in increasing mobility with shorter hospital stays and better overall patient satisfaction.
He acknowledges that there needs to be further work to provide clearer data from human clinical studies, as clear evidence is difficult to come by in small sample sizes. This is why dialogue and information sharing between practitioners is important to him.
Tools to consider
To support a strong interdisciplinary perspective and to keep focused on providing a wholistic approach to pain management, Roca Ruiz reiterates the importance of maintaining a mindset that addresses the whole timeline of the patient’s surgical journey: pre-surgery, during the surgery and postoperative.
Returning to his experience with TKA, Roca Ruiz maintains that without focused attention on managing peripheral issues of the surgical timeline, a baseline of between 11% and 20% of patients will be dissatisfied with some element of the procedure, especially when it comes to pain. To reduce this risk, he recommends a tactical list of the key priorities on which to focus at the various phases of the patient’s surgical journey to improve patient expectations, patient pain and overall patient outcomes.
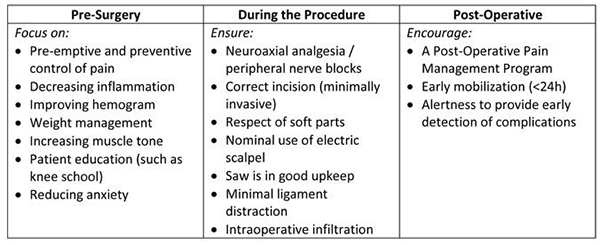 This perspective provides simplified awareness of three pillars of the patient journey through the surgical intervention. According to Roca Ruiz, obviously orthopaedic surgeons and traumatologists will be heavily interested in building their skills and focusing on their activities during the surgical procedure, but he suggests balancing this view in such a way that provides the perspective that the pre- and post-surgical steps are just as important to influencing the best patient outcomes as the care involved in precision performance during the procedure.
This perspective provides simplified awareness of three pillars of the patient journey through the surgical intervention. According to Roca Ruiz, obviously orthopaedic surgeons and traumatologists will be heavily interested in building their skills and focusing on their activities during the surgical procedure, but he suggests balancing this view in such a way that provides the perspective that the pre- and post-surgical steps are just as important to influencing the best patient outcomes as the care involved in precision performance during the procedure.
Roca Ruiz mentions that almost 30% of patients awaiting surgery for osteoarthritis of the knee present neuropathic pain. Aware of this fact in these patients and others, orthopaedic surgeons should be actively engaged in correctly diagnosing problems to best prescribe the most impactful treatment options. As part of this process, he emphasizes an enlarged perspective of the supporting professional team that is essential to enhancing overall surgical success and improved postoperative pain management. This team includes the nursing staff, social workers and physical therapists who support in preoperative education and exercises that serve as non-pharmacological analgesic supports that will assist in overall long-term pain management and mobilization results.
Anesthetists are also key partners for orthopaedic surgeons and traumatologists, not only during the surgical procedure, but before and following the intervention. Only with a solid team and an enlarged global vision of the patient’s surgical journey and pain management plan can responsible practitioners provide top quality care to their patients.
One example of a practice that balances this perspective, according to Roca Ruiz, is fast-track rehabilitation after TKA. In implementing an effective fast-track programme, an interdisciplinary team focused on all phases of the patient surgical journey is essential. Fast-track rehabilitation managed with this global perspective, according to Roca Ruiz, shows great results for patients not only in the return to proper functioning, but also with regard to incorporating preventive analgesia that directly impacts lengths of stays, measurements on the WOMAC index, and postoperative analgesic drug consumption. With programmes for fast-track rehabilitation, various disciplines must work together to ensure pre-surgical and intra-surgical pharmacological and anesthetic infiltration, as well as follow-up with the results of increasingly effective postoperative pain management programmes that provide overall better patient results.
Roca Ruiz notes that taking greater care to include central sensitisation in the diagnostic spectrum of patients with “unexplained” pain is one way to be a better practitioner with regard to preventive analgesia and its impact on postoperative pain. Referring to Nijs (2014), he points out that central sensitisation is present in a variety of chronic pain disorders, including whiplash, temporomandibular disorders, lower back pain, osteoarthritis, fibromyalgia, headache, lateral epicondylalgia and others. Even though the medical community continues to understand more regarding the mechanisms involved in central sensitisation pain, its treatment is still a challenging issue. Key to this treatment, however, is for orthopaedic surgeons and traumatologists to ensure global thinking with interdisciplinary teams surrounding their patient’s pain pre-surgically, during the procedure, and postoperatively.
Further reading
To build understanding of preventive analgesia in the community of orthopaedics and traumatology, Roca Ruiz shares some suggested reading:
Concerning the correlation of presurgical pain with postoperative pain
- Judge A, et al. Rheumatology (Oxford, England). 2012;51(10):1804-1813.
- Puolakka PA, et al. Eur J Anaesthesiol. 2010;doi:10.1097/EJA.0b013e328335b31c.
- Rat AC, et al. Arthritis Care Res (Hoboken). 2010;doi:10.1002/acr.20014.
- Jones CA, et al. Arch Intern Med. 2001;doi:10.1001/archinte.161.3.454.
- Strategies and predictors of success for function and mobility.
- Fortin PR. Arthritis Rheum.1999;doi:10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R.
- Am J Orthop. 2016; 45 (7): S1-S7.
- Hernándeza C, et al. Reumatol Clin. 2015;doi:10.1016 / j.reuma.2014.12.008.
- Kalkman CJ, et al. Pain. 2003;105(3):415-423.
- Lewis GN, et al. Br J Anaesth. 2015;doi:10.1093/bja/aeu441.
- Puolakka M, et al. Eur J Anaesthesiol.2010;doi:10.1097EJA.0b013e328335b31c.
Further references
- Bourne RB, et al. Clin Orthop Relat Res. 2010;doi:10.1007/s11999-009-1119-9.
- Herrero Gracia M, et al. Rev Soc Andaluza Traumatoi Ortop. 2002;22:148–153.
- Nijs J, et al. Expert Opin. Pharmacother.2014.doi:10.1517/14656566.2014.925446.
- Noble PC, et al. Clin Orthop Relat Res. 2006;452:35-43.
Engage in the Post-Operative Pain Management discussion
Engage in the Post-Operative Pain Management discussion by using the following hashtags on Twitter, Facebook and LinkedIn:
- #painmanagement
- #POPM
- #changepain
For more information
As the platform organisation linking Europe’s national orthopaedic associations, the European Federation of National Associations of Orthopaedics and Traumatology partners with Grünenthal to raise further awareness of the unmet needs in postoperative pain management (POPM) and to develop solutions that improve POPM across Europe.
Over the next 6 months, we will involve pain experts from across Europe in interviews, debates and other discussions to generate a better understanding of physicians’ and patients’ perspectives. The goal of this series is to communicate best practices and increase discussion on POPM in general.
Burson-Marsteller, established in 1953, is a leading global public relations and communications firm, and the EFORT-mandated press agency for the POPM awareness campaign. All articles published herein respect the third-party content policy of EFORT as published on our website.
For any articles related inquiries, please contact media@efort.org.


